Causes of chest pain
The causes of chest pain can range from harmless to imminently life-threatening. This makes it one of the most important symptoms for medics to be able to interpret quickly. Chest pain is often considered a medical emergency until cardiac (heart-related) causes are excluded. Having a differential diagnosis in mind helps medics take a history, examine, and choose investigations to solve the case.
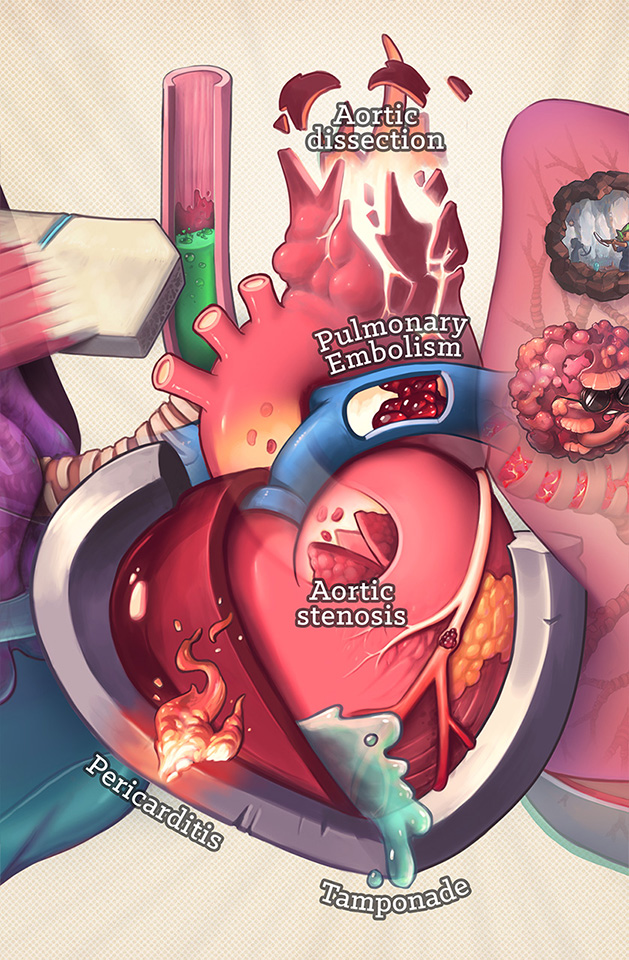
Below is my illustrated differential diagnosis of causes medics should be aware of.
Causes of chest pain
When there are a lot of diagnoses to remember it is often helpful to divide them into categories. One way to do this is anatomically:
Cardiac
Respiratory
Gastrointestinal
Musculoskeletal
Cardiac
Acute coronary syndrome (ACS)
ACS describes reduced blood flow to the heart muscle. People often report pain as being tight, “like a band across my chest”, and heavy “like an elephant sitting on my chest”. Pain can radiate from the chest to the neck, jaw, left arm, and back. Associated symptoms include nausea, vomiting, shortness of breath, sweating, and a sense of impending doom.
ACS can be caused by narrowed blood vessels, e.g. due to atherosclerosis (fat deposit in artery walls), or vasospasm e.g. via cocaine use. Angina is a common type of chest pain brought on by exertion when the hearts blood vessels are narrowed by atherosclerosis. The heart can’t keep up with the demand for more activity. It is quickly relieved by rest and medication. A myocardial infarction (“heart attack") results from prolonged lack of blood flow to the heart, causing damage and death of cardiac tissue which can kill. A heart attack can present unusually, e.g. without pain, in diseases like diabetes which can alter nerve sensation throughout the body.
Note that anaemia and blood loss e.g. following trauma, or during surgery, can put increased strain on the heart too, as there are less red blood cells to feed it oxygen. This is called a ‘type-2 myocardial infarction’.
Cardiac causes of chest pain (close up) medical illustration by Dr Ciléin Kearns (Artibiotics)
Aortic stenosis (AS)
The aortic valve sits between the left ventricle (main chamber) of the heart, and aorta (the main blood vessel leaving the heart to carry oxygenated blood around the body). Over time the ‘leafs’ of the valve can thicken and become less flexible (stenosed), reducing its ability to open and close. This means less blood flows through it when open, and blood leaks out when it should be closed (causing a murmur that can be heard with a stethoscope). This affects the pressure the heart can generate to pump blood, reducing the effectiveness of each beat.
Similar to ACS, a stenosed aortic valve (AS) reduces blood flow from the heart to the bodies tissues. The effects of AS are more pronounced when the demand for blood increases on exertion. When severe this can cause chest pain and syncope (fainting) on exertion. An ‘ejection systolic murmur’ can be heard with a stethoscope from the top right sternal edge (location of the valve) radiating to the right carotid in the neck (the direction of blood flow).
Pericarditis
This is inflammation of the pericardium, a fibrous bag around the heart. It can follow a viral infection, heart attack, or heart surgery, but the cause is often unknown. Pericarditis causes a sharp, stabbing, knife-like pain, which may be made worse on deep breathing or by lying down. The pain may be relieved by leaning forwards. A pericardial friction rub may be heard on auscultation.
Aortic aneurysm and dissection
The blood is at its highest pressure in the aorta, the biggest artery it is pumped through after leaving the heart. A tear in the inner wall is called an aortic dissection. It usually happens because the wall has been weakened over time by uncontrolled high blood pressure, trauma, or a genetic condition which affects its structural integrity. A sudden dissection can kill, and fast. The chest pain occurs suddenly and is often described as tearing, ripping, or shearing. It may radiate up to the neck, through to the back, and down to the stomach. On examination, a patient may have unequal radial pulses at the wrist if the tear occurs between the branches off the aorta to each arm (the branch after the tear is weaker).
Although complete rupture can occur (which allows blood to leak into the chest cavity), it is more common that blood peels apart the layers of the aorta wall and collects here in a ‘false lumen’ (the ‘true’ lumen being the channel blood usually travels). This ballooning of the false lumen is called an aortic aneurysm. Aneurysms cause all sorts of problems:
Haemodynamic instability: with blood leaking from an important high pressure system, the heart may not be able to compensate for lost volume and pump enough blood to the other tissues.
Extension: aneurysms can extend right along the aorta from the chest to the pelvis. This can occur at the time of the initial dissection, or progress over time if not managed. Extension causes particular problems at branching points of the vessel, where the blood supply to the branch can be compromised, or rely on the false lumen (which complicates surgery).
Mass effect: the size of the aneurysm can compress tissues around it such as other blood vessels, the heart and lungs, digestive tract, etc.
Rupture & death: the wall of an aneurysm is stretched and weaker than a healthy vessel. It is sometimes thought of as a ‘ticking time bomb’ as it can burst. However, this risk is proportional to the size of aneurysm so surgeons often recommend monitoring until the ‘risk of rupture’ outweighs the risk of major surgery to repair.
Respiratory
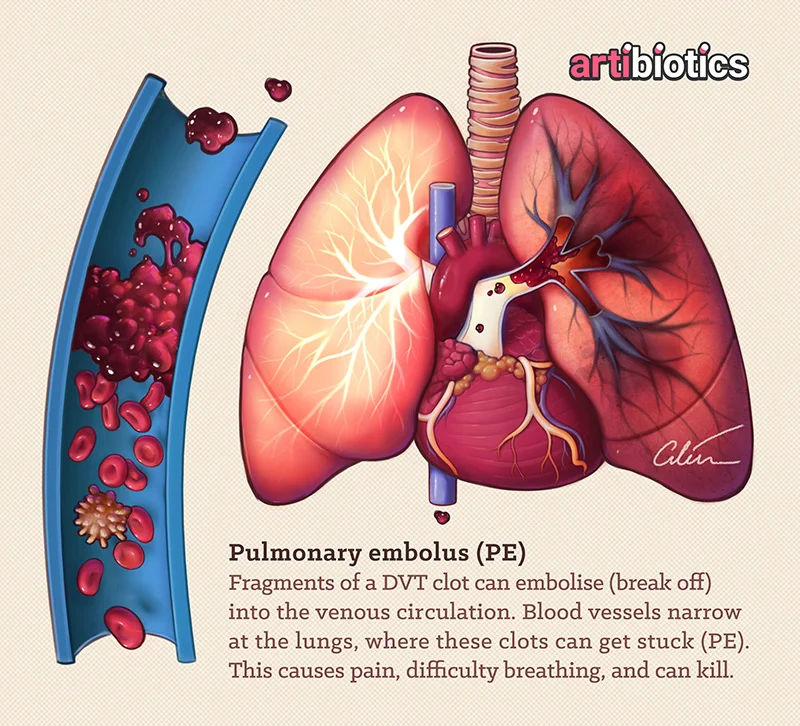
Pulmonary embolism (PE)
Clots that form in veins often get stuck in the artery leaving the heart and branching into the lungs (pulmonary artery). Until this point, the size of the veins and heart chambers it has travelled through will have been increasing, but the path suddenly narrows as vessels branch into the lungs. A clot here can be catastrophic as it cuts off circulation to all or part of one or both lungs (depending on the size and how far it travels before sticking). Reduced blood flow through the lung tissue makes that tissue less effective at breathing, a bit like suffocating from the inside. People can feel pleuritic chest pain (worse on deep breaths), breathless, and have worse symptoms on exertion. A deep vein thrombosis (DVT) is sometimes the herald of a PE, we take leg clots so seriously to prevent them breaking off to become the more life-threatening PE.
Pulmonary Embolism medical illustration by Dr Ciléin Kearns (Artibiotics)
Pneumothorax
A pneumothorax is a disruption in the lining of the lung which allows an air leak. This can act like a one-way valve so air accumulates outside the lung in the chest, but cannot escape. It can be life threatening as this mass of air expands, eventually crushing the heart (so it can’t pump blood) and lungs (preventing breathing). A pneumothorax can occur spontaneously, often in smokers with underlying respiratory disease e.g. COPD, and also in tall, thin, young men.
Tension pneumothorax medical illustration by Dr Ciléin Kearns (Artibiotics)
Haemo-/hydro-/pyelothorax
These conditions describe blood, fluid, and pus accumulation outside the lung which act similarly to a pneumothorax in crushing the lung and chest contents.
Chest infections
Basal pneumonia and tuberculosis are two examples of chest infections which can cause referred chest pain.
Tuberculosis ‘cavitating lesion’, medical illustration by Dr Ciléin Kearns (Artibiotics)
Bronchitis and Asthma
Both conditions involve inflammation of the airways, coughing, and increased infections, all of which can cause chest pain.
Asthmatic vs healthy airways closeup medical illustration by Dr Ciléin Kearns (Artibiotics).
Lung cancer
This can cause chest pain by pressure on, and invasion into, nearby structures e.g. nerves.
Lung cancer medical illustration by Dr Ciléin Kearns (Artibiotics).
Referred gastrointestinal pain
Gastro-oesophageal reflux disease (GORD) describes acid leaking from the stomach back up the oesophagus due to a weakened/relaxed sphincter at the stomachs opening. It can cause a burning sensation along this tract between mouth and stomach (ie chest). This is worse on lying down where gravity can encourage this backing-up, and also after eating when the stomach is fuller.
Other important causes include peptic and duodenal ulcers which can perforate and require surgical intervention. Many causes of abdominal pain can result in referred pain to the chest so check out my illustrated ddx for this symptom for a deeper look!
Referred stomach pain, closeup by Dr Ciléin Kearns (Artibiotics)
Musculoskeletal (MSK pain)
This category is often a diagnosis of exclusion, ie, once all the scarier things have been excluded. “MSK pain” catch-all term that encompasses any injury to the muscle, tendons, bones, and ligaments. A strain on any combination of these can result in inflammation and pain which is worsened by activity involving these structures (or palpating them!).
Costochondritis and Tietze’s syndrome
The costal cartilage is a tissue connecting the ribs to the sternum bone in the center of the chest. Costochondritis describes pain where the bone and cartilage meet here. This can come in flares provoked by activity, deep breathing, or coughing, and may affect multiple ribs. Sometimes the cartilage is also painfully swollen; this is called Tietze’s syndrome. The pain may be worsened by palpating the affected cartilage.
Rib fracture
People usually report a history of a trauma to cause these. A significant rib fracture can provoke a pneumothorax or bleed in the chest.
Psychological
Anxiety / panic attack / somatisation
A panic attack should be a diagnosis of exclusion when someone presents with chest pain. Psychological distress can manifest with physical symptoms largely via the autonomic nervous system. This “flight or fight” response is often triggered inappropriately in todays world. Anxiety was presumably an evolutionary advantage at one stage when sabre-toothed tigers were around every corner, and neighbouring clans out to kill you every day. Being on edge had a survival benefit. Today however it has little value for the majority of us…
Causes of chest pain
And that’s it! This visual isn’t exhaustive; are there any other important diagnoses you think are important to include?
This art is from my “Medical Mentalism” series.